The liver cancer challenge
Why precision medicine?
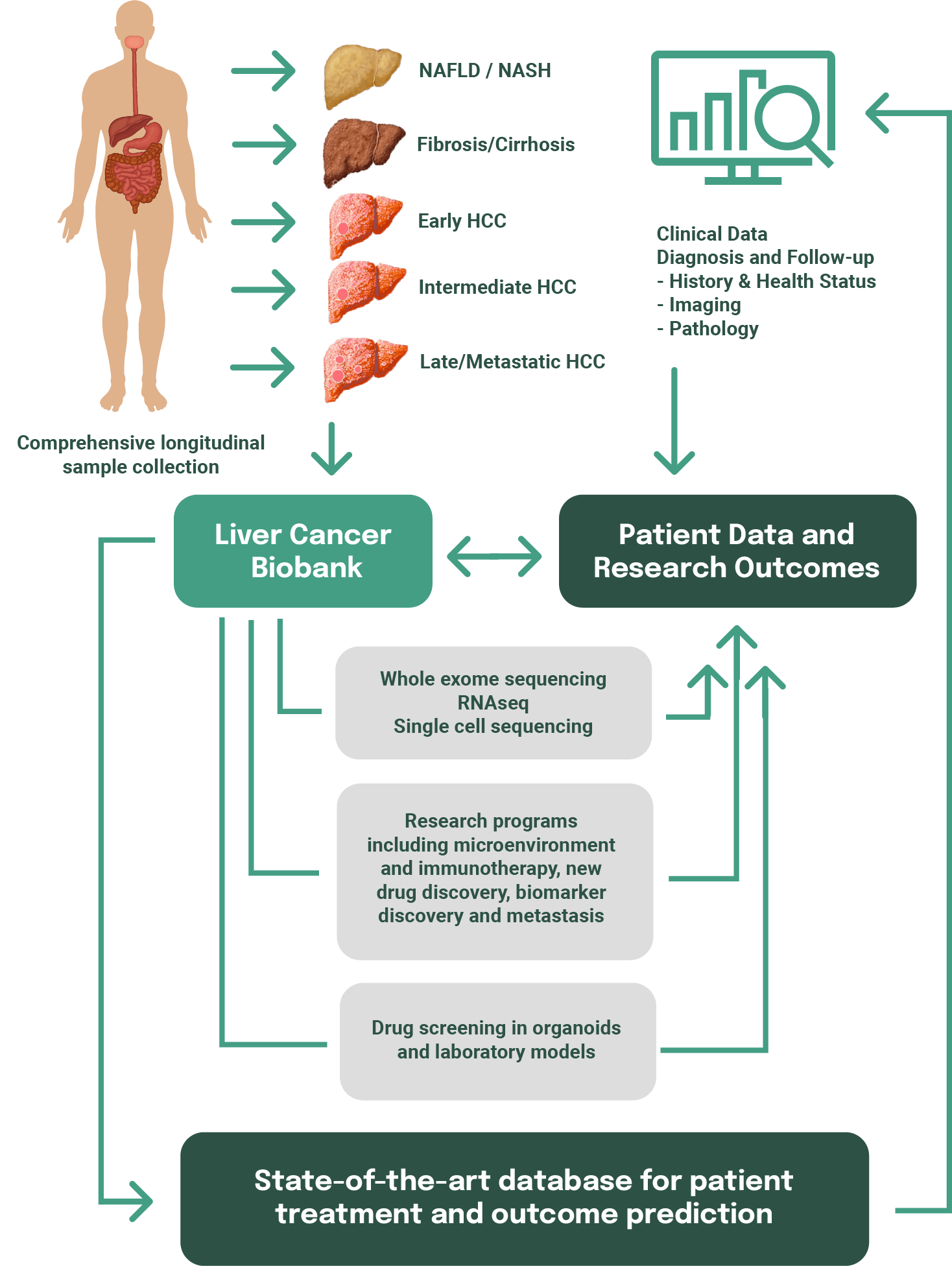
Precision medicine allows a patient’s treatment to be customised. Precision medicine starts by combining genomic data, that is data about the genes within the cancer, with patient information such as treatment response, development of drug resistance and overall outcome. Using these data from hundreds of individuals, we develop molecular profiles that correlate with different disease stages (ie from NAFLD/fatty liver disease to HCC) and different treatment responses.
These molecular profiles can then be used to predict an individual patient’s cancer progression and help clinicians determine the best treatment options.
Tissue donated by patients as part of this program will help us generate the molecular profiles required to develop a precision medicine approach for liver cancer. These data will significantly contrbute to improving treatment for future patients.
Our Research
The Liver Cancer Collaborative (LCC) has partnered with the Perkins Cancer Biobank to build one of the world’s most extensive tissue repositories for liver cancer. LCC clinicians and scientists are collecting samples of blood, healthy tissue and cancer tissue from hundreds of participants across their cancer journey. These samples will provide a wealth of information about how liver cancer develops and will enable identification of biomarkers that have the potential to predict treatment response, drug resistance, recurrence and outcome. Samples in the LCC biorepository are used across 3 major research programs.